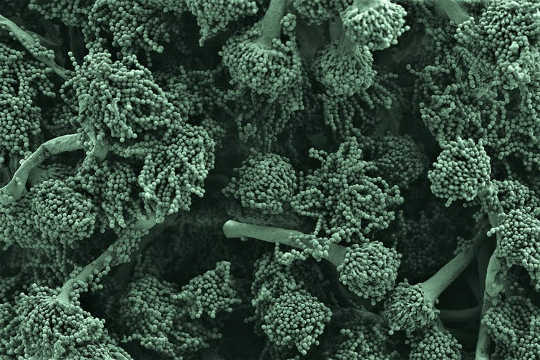
A microscopy image of Aspergillus fumigatus fungus, one of the biggest killers of patients with weak immune systems. Mark Stappers/Kevin Mackenzie, Author provided
Fungi are ubiquitous in nature. No one really knows how many species of fungi there are – one estimate is between 2.2m and 3.8m – and of those species only 120,000 have been documented. Fungi and moulds encompass a dizzying range of physical forms and attributes, living in both temperate environments and in extremes of hot, cold, or in the depths of the ocean.
Most play a vital but unseen role breaking down plant matter and redistributing nutrients through the soil. Some are good to eat – yeasts, for example, are integral to creating bread, beer and other foodstuffs that have shaped societies and cultures over many centuries. But many others are toxic, for example the poisonous death cap. Fungi have had on occasion wrought terrible effects on the natural world: the chytrid fungus epidemic has decimated amphibian populations worldwide, driving species towards extinction, and other fungi have attacked staple food crops, endangering food security.
But less well appreciated is the influence of fungal infections on humans, which has increased substantially over the last few decades. There is a rising tide of fungi invisible to the eye that causes us harm, whether we can see it or not.
Fungi are widespread and persistent
Around 25% of the world’s population contracts a fungal infection of the hair, skin or nails each year, such as athlete’s foot. Most women suffer from at least one fungal infection such as thrush, and a significant proportion experience these regularly. While the majority of these so-called “superficial” fungal infections are relatively easy to diagnose and treat, a few cause debilitating and disfiguring infections for which there are very limited treatment options. And resistance to drugs is growing.
They’re lethal
Incredibly, invasive fungal infections kill three times more people than malaria. Only a few fungi can cause fatal diseases in healthy people, and these are generally rare and occur only in certain geographic regions such as in South America. But of greater concern are infections of normally harmless fungi that occur in those with weakened immune systems. For example, modern immunosuppressive drugs used for organ transplants or for treating HIV/AIDS, have seen huge increases in the number of people infected.
It is scary how lethal these infections can be, with a mortality rate often exceeding 50%. Recent statistics suggest that at least 1.6m people die every year as a result – roughly equivalent to the number of deaths from tuberculosis worldwide. Like other pathogens, the majority of related deaths occur in low and middle income countries where therapeutic options are limited.
Hard to diagnose, hard to treat
Fungal infections are very difficult to diagnose and treat, and this is partly why invasive fungal diseases have such a high mortality rate. With few exceptions, current approaches to diagnose fungal infections are fraught with issues around the ability to accurately detect them. This leads to delays in starting treatment, often with fatal consequences.
Our therapeutic arsenal is also limited. We have comparatively few drugs, and many of these are toxic or interact badly with other commonly used drugs. They may only be effective on a narrow spectrum of fungi, or may be problematic to administer. It is telling that there is not a single vaccine against fungal infections in current clinical use. Worryingly, drug resistance is increasing and there are very few new drugs in clinical development. And many key antifungal drugs are also unaffordable or unavailable in the low and middle income countries where they are needed most.
Linked to diseases we don’t understand
Fungi are increasingly linked to myriad human ailments, such as allergic and asthmatic diseases that affect millions of people. Fungi cause over a million eye infections every year, many of which result in blindness. Recent evidence, mostly from animal models, suggests that alterations in the fungal components of the gut can affect the severity of gastric ulcers, ulcerative colitis, Crohn’s disease, food allergies, and even alcoholic liver disease. There are also a few reports that link fungi to neurological disorders such as Alzheimer’s disease.
And we’re not paying enough attention
Our ability to tackle fungal diseases is severely hampered by a worldwide lack of scientists and clinicians working in this area. This lack of capacity is particularly severe in the developing world, which suffers the greatest burden of disease.
Compared to huge amount of research done on infectious bacteria or viruses, most fungal infection research is conducted by small groups or individuals. There are only a handful of larger research centres around the world, of which the MRC Centre for Medical Mycology in Aberdeen is one. Fungus research funding accounts for less than 3% of the infectious disease budgets of major international funders (at least in the UK and US), which reflects the lack of funding applications submitted.
![]() If we are to attract experts to build the increased research capacity that is desperately needed to tackle these challenges, a greater awareness of the growing health harms caused by fungal infections is vital.
If we are to attract experts to build the increased research capacity that is desperately needed to tackle these challenges, a greater awareness of the growing health harms caused by fungal infections is vital.
About The Author
Gordon Brown, 6th Century Chair in Immunology, Director, MRC Centre for Medical Mycology, University of Aberdeen
This article was originally published on The Conversation. Read the original article.
Related Books
at InnerSelf Market and Amazon